Organisms and pathogens have been evolving together since the beginning of life on earth. Humans have always been exposed to infectious organisms and sometimes they kill us and sometimes we adapt and fight them off. What determines what pathogens kill us, why are some easier to fight off than others?
Topics covered:
- How viruses infect cells
- Stages of infection
- How our immune system responds
- Innate immune cells
- Adaptive immune cells
- Why do we keep getting colds – how viruses change over time
- Factors that affect the severity of infection
How Viruses Infect Cells
Viruses require a specific cell receptor to bind to and then infect a cell. For example:
- Hepatitis infects liver cells
- Epstein Barr (mono) infects B cells
- HIV infects T cells and monocytes (white blood cells) – making people immunocompromised so death can occur from any kind of infection
- Cold and flu viruses infect the epithelial cells that line our respiratory system
For viruses to be able to bind they have to have proteins on their coat and they can have a range of structures; generally most viruses that infect humans have a spherical shape where their genetic material is inside a protein envelop. Here are some example images from Virus Particle Explorer. All the little sticking out parts are antigens that can bind to our cells or are recognized by our immune cells.

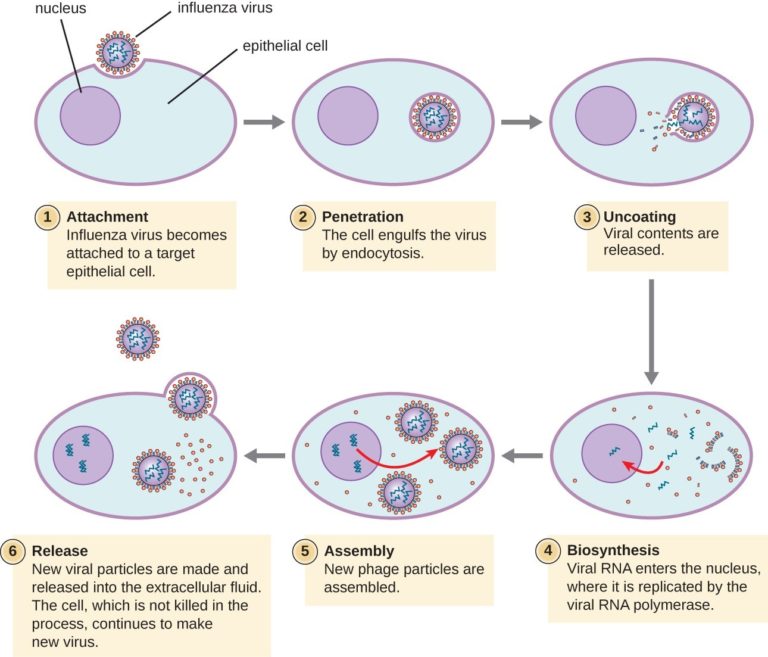
Virus particles have several stages of infection:
- Bind to receptors on our cells
- Our cells take them in
- Viruses hijack our cellular equipment (organelles) and replicate themselves
- New virus particles are released from the cell and may or may not kill our cells in the process
- New virus particles spread to more cells
This example is showing influenza but common cold viruses like coronavirus infect cells a similar way, they just have different surface proteins that bind to a different receptor.
How our immune system responds to viral infections
We have innate (non-specific) and as adaptive (specific) mechanisms for dealing with infections. We have a variety of different types of immune cells that recognize and kill various types of pathogens. When we have a viral infection, we have several mechanisms for generally preventing microbe entry or generally killing microbes such as:
- Skin and epithelial cell barrier – act as physical barrier between the inside of our body and the external environment, damage to the barrier gives organisms and way in
- Mucus – traps organisms, then we cough and get rid of them
- Cilia – hair-like structures in the respiratory tract that move mucus-trapped organisms up to be coughed or sneezed out
- Antimicrobial chemicals like lysozyme in our saliva and tears that can kill some types of bacteria
- Hydrochloric acid in our stomach kills many organisms we swallow
- Microflora – our symbiotic bacteria that help to kill pathogens, on the surface of our skin and in our digestive tract – microflora also help to regulate our immune system
- Interferons – chemicals that are produced by virus-infected cells that alert nearby cells to shut down replication machinery
- Inflammatory response – dilation of blood vessels to bring in more nutrients to infected area, infiltration of many more immune cells to fight pathogens, this causes swelling and pain of infected area – makes it harder to breath, chest feels tight and sore, throat may be sore
- Fever – temperature response can be initiated by some pathogens that trigger the hypothalamus to increase body temperature in attempt to increase the immune system metabolism and to kill pathogens that are adapted to replicate at normal body
Innate Immune Cells
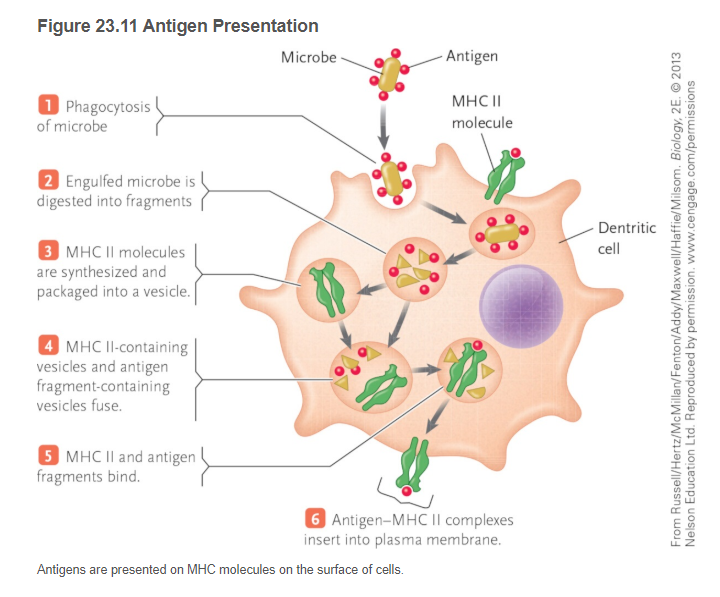
Cells that recognize foreign microbes and kill them (like neutrophils) or engulf them (like macrophages or dendritic cells). Macrophages that engulf virus particles will “present” pieces of those viruses on their cell surface, called antigen presentation, and they carry those bits of antigens to the lymph nodes where they activate our specific immune cells, the B cells and the T cells. The diagram below is from my textbook and it shows how innate immune cells present viral particles on their surface – step 6 below is how we activate B cells and T cells in the lymph nodes or spleen.
Adaptive immune cells
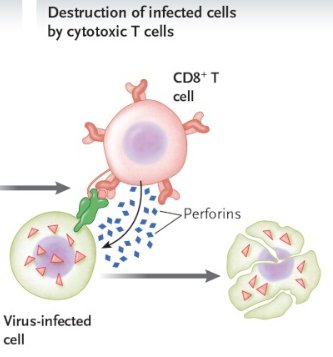
The main adaptive immune cells that kill viruses are our cytotoxic T cells. Once they are activated by antigen-presenting cells, they are like snipers. They proliferate and specifically target our own cells that are infected by that specific virus that was presented by the dendritic cell and they kill them. It is important to note that different T cells (CD8+ T cells) are activated for each different kind of pathogen that infects us. This also contributes to the inflammation and soreness or aching that goes along with a cold or flu; our immune system is killing our own cells that are infected to stop the viruses from being able to replicate.
A very important KEY component of how our immune system deals with infections is the production of MEMORY cells after the infection dies down. We have lymph nodes that are loaded with memory cells from past infections! Then, when we come in contact with that pathogen again, our memory cells can kick in so rapidly and kill it before we even notice anything is going on. Our immune system is constantly dealing with pathogens but we only get symptoms from new things!
So why do we keep getting common colds if we have memory cells?
We get sick from common colds every year because virus particles change slightly all the time. The surface proteins that our immune cells recognize can be altered because every time they replicate, tiny changes can occur in their DNA and that changes those surface proteins. When new surface proteins arise, then we have to activate new T cells with different receptors and then make new memory cells.
When common cold or flu viruses only alter a little bit each year, then we have some memory cells that recognize some antigens and we can fight it off with the usual minor symptoms of sneezing and coughing and feeling crappy for a week or so. Sometimes colds are very minor then we know we probably have a lot more memory cells from previous infections and the virus is only slightly different from what we have been exposed to before.
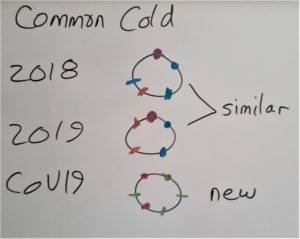
When a virus can replicate quickly, and when it can infect more than one species, then mutations happen faster! Then virus particles can become very different very quickly. That is what happened with COVID19. Because it can replicate in other species like bats as well as humans, it has more NEW surface antigens and therefore we don’t have memory cells and our immune system has to work a whole lot harder to kill it….but then we will make memory cells for this infection too. Let’s suppose the coloured dots represent different surface proteins.
The harder our immune system has to work to fight off a new pathogen, the more symptoms we get. The pain, swelling, fever, aching, coughing, wheezing etc symptoms are from our immune system reacting and trying to kill the infection. Our immune system has to work harder if the pathogen has a lot of new surface antigens or if your body has taken in a larger concentration of virus particles….this is why washing your hands and not touching your face is important, it reduces the number of pathogens your immune system has to deal with.
Factors that affect the severity of infection
- Concentration of virus particles – pathogens can spread from person to person much easier and in much higher amounts when people are grouped together in large numbers in a space – one reason why we get sick less in the summer, because people spend more time outside father away from each other and it makes it harder for pathogens to get around – also why we quarantine and close large events to help prevent rapid transmission
- People that are most likely to die from infections have a weak immune system and can’t kill the virus particles or infected cells faster than the virus can replicate – most common vulnerable populations are very old and very young – young people don’t have as much memory cell population yet so more infections are new, also people taking immune inhibitor medications
- People that smoke or vape have damage cilia and resident immune cells and are unable to clear respiratory pathogens
- People that have other health conditions such as cardiovascular disease and diabetes have a significantly reduced ability to activate all aspects of an immune response that help to kill the infection
- Not enough protein in the diet – the immune system requires a huge supply of amino acids to produce antibodies and to proliferate all the immune cells required to fight the infection, and we need more protein to rebuild cells after they have been damaged….by the viruses as well as our own immune system
- Lack of sleep or excess stress – sleep deprivation is a major stimulus for the production of cortisol, a stress hormone that inhibits the immune system! Get enough sleep, nap and sleep a lot if you have any symptoms, your immune system needs all the energy it can get
- Excess iron – do not take iron supplements when you are sick, microbes feed off of iron and use it for replicating. In fact, when you are sick, your liver stops putting iron into the blood until the infection is gone.
- Not enough vitamin A – viruses tend to cause our body to be depleted in vitamin A, our immune system requires a LOT of vitamin A to replicate all the immune cells needed to fight the infection
- Opportunistic infections – when your immune system is very busy fighting off something new, other sneaky infections can make their way in and replicate and cause a secondary infection, such as pneumonia. There are viral and bacterial pneumonia organisms and they can overwhelm the immune system; eventually there are more pathogens than the body can deal with and death can occur.