The lining of our small intestine is where we absorb the nutrients we have digested. It is very important to have a healthy intestinal barrier so that only fully digested nutrients enter our bloodstream. If undigested large molecules leave the intestine and get into the interstitial space and bloodstream then an inflammatory response is triggered. Having continual intestinal inflammation will increase overall systemic inflammation in the rest of the body and will exacerbate any inflammatory condition. The key to decreasing chronic inflammatory conditions is to first make sure your intestinal lining is healthy.
Chronic conditions that are caused by or exacerbated by inflammation
- Cardiovascular disease
- Alzheimer’s and dementia
- Autoimmune diseases – arthritis, crohn’s, colitis, lupus, Hashimito’s, Grave’s, Celiac, myasthenia gravis, multiple sclerosis, psoriasis, etc
- Diabetes
- Mood disorders
- Various skin conditions
- Allergies
- Asthma
- Osteoarthritis
- Cancers
- Fibromyalgia
- Metabolic syndrome
- Obesity
- Irritable bowel syndrome
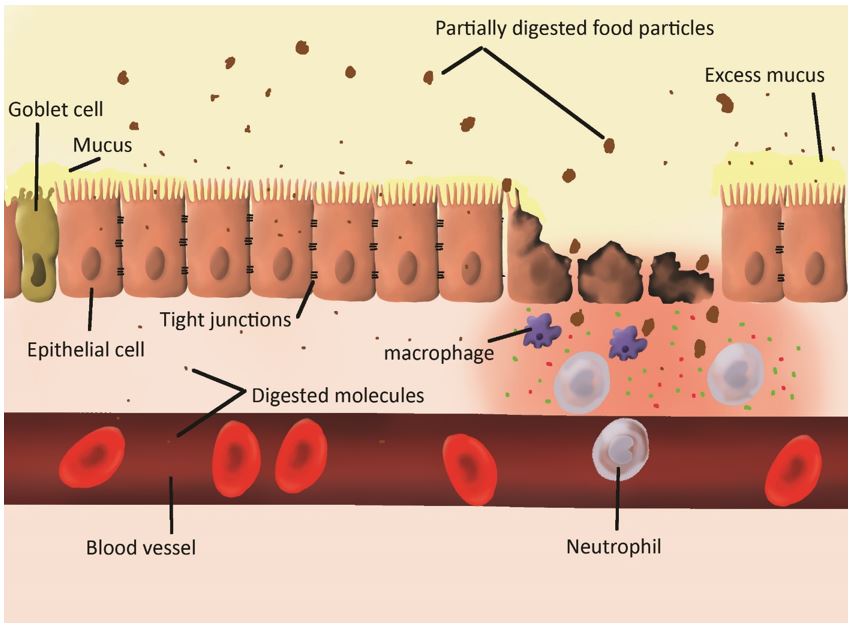
As you can see, many diseases and conditions are affected by inflammation, and the gut in the first place that needs to heal. Check out the following diagram (that I drew in Photoshop, so fun learning to draw super cool images so I can explain important concepts J) I drew this because I believe digestive health is the root cause of many conditions and a lot of people don’t know the significance of taking care of their digestive system for preventing chronic diseases. In this diagram you can see a section of small intestine lining with the left side showing a healthy lining and the right side showing damaged lining. Nobody has 100% healthy gut lining. The goal is to minimize the damaged areas as much as possible and allow the intestine to heal. Luckily, the intestine can heal very quickly! We replace epithelial cells every 3 days, so it is possible to turn things around in a relatively short period of time depending on how much of your intestine looks more like the right side of this diagram.
Important physiology about how your small intestine lining works
- The beige cells with “hair” are the epithelial cells where absorption of nutrients occurs. The top part of the diagram is the lumen (inside) of your intestine where food is being digested with enzymes so that proteins become amino acids, carbohydrates become glucose and fructose, and fats become fatty acids and glycerol. The “hair” is microvilli that increase the surface area of absorption so that we can get more nutrients out of our food.
- The epithelial cells form a barrier. See the tight junctions between the cells; they prevent undigested large macromolecules from moving between the cells and entering into the interstitial space and bloodstream.
- Goblet cells produce mucus that help to protect the epithelial cells from being digested by the enzymes that are digesting the food. We want to have a nice thin layer so that the epithelial cells are protected but not too much….like the far right side, because excessive mucus prevents the absorption of nutrients.
- Damaged epithelial cells let undigested molecules cross the barrier. When the tight junctions are broken down or some of the epithelial cells become damaged, then large molecules enter and stimulate the immune system.
- Immune cells like macrophages and neutrophils secrete inflammatory cytokines in order to attack the large molecules. Cytokines attract more immune cells and then the immune cells react to the large molecules as though they are pathogens. Immune cells cause a lot of damage to normal healthy cells and it can cause a chain reaction of inflammation. The inflammatory response also causes goblet cells to increase mucus production in attempt to reduce damage to the gut lining but this also has the side effect of reducing nutrient absorption.
- Reduced absorption of micronutrients, vitamins and minerals, contributes to many of the symptoms associated with damaged intestinal lining.
This damaged intestinal lining is sometimes called “leaky gut”. It can trigger reactions to certain foods causing a food “sensitivity”. It not the same as an allergic reaction that cause anaphylaxis but food sensitivities stimulate the immune cells and cause symptoms.
See article – What is inflammation?
How can you tell if your intestinal lining is damaged?
Symptoms can de varied and diverse but the following is a list of the main symptoms many people might experience.
- Fatigue – this seems like an unrelated symptom but generalized fatigue (which can be caused by many things) is a primary symptoms of intestinal inflammation; the immune system uses a lot of energy
- Difficulty concentrating (many causes for this as well but is a very common symptom in people with damaged intestinal lining)
- Bloating
- Gas
- Cramping or abdominal pain after eating
- Feeling of indigestion, fullness that lasts a long time after eating, that feeling when you just want to lay down after a meal
- Nausea
- Constipation or diarrhea or alternating abnormal bowel movements
- Seeing undigested foods in your bowel movements (except corn, if you see corn that is normal, nobody breaks that down ha)
- Mucus in bowel movements
- Skin problems such as rashes, eczema, or acne
- Headaches
- Moodiness and irritability – will occur with any kind of inflammation due to the secretion of cytokines
- Joint and muscle aches and pains – many people blame “aging” but this is very highly connected with inflammatory conditions
- Food sensitivities – having issues with any specific foods that is not an allergic reaction is definitely an indication that the gut lining is damaged.
What causes the intestinal lining to break down?
The following is a list of the most common causes of breakdown of the tight junctions, cause epithelial cell death or dysfunction, malabsorption, or excess mucus production.
- Ibuprofen – directly causes break down of tight junctions, so make sure to only use Ibuprofen/ Advil sparingly and not on a regular basis
- Alcohol – Although alcohol in moderation (1-2 drinks per day) is considered to be “healthy” and helps to reduce blood pressure and stress, daily consumption can be tough on your intestinal lining, especially if you already have obvious symptoms. Binge drinking is extremely hard on the intestinal lining and should be avoided.
- Sugar – Sugar is very pro-inflammatory. If you have one or more inflammatory issues (many people have more than one) then quitting sugar should be high on your list of priorities.
- Trans fat – also very pro-inflammatory and avoiding processed oils such as canola, vegetable, corn, soybean, and anything hydrogenated or modified is essential.
- Stress – Cortisol is a stress hormone that decreases immune regulation and perpetuates inflammation. Stress also greatly and directly inhibits all digestive functions. Make sure to eat in a relaxed environment so that your parasympathetic nervous system can stimulate digestive enzyme secretion, intestinal motility, and blood flow to the intestines and liver. Chronic stress is one the worst things for digestive health.
See article – How cortisol impacts your health